Remittance Advice Report
Note that Electronic Remittance Advices are only available from Panacea version 7.1 onwards.
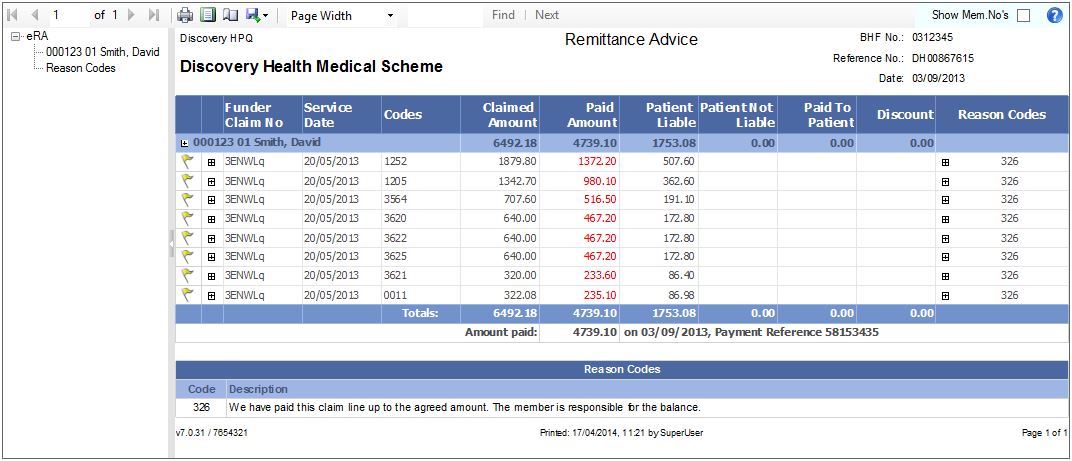
Panacea's eRA report looks like this:
Click
here
for information on working with reports.
The eRA report is intentionally designed to look like "traditional" paper-based Remittance Advices that you have received from the various medical aids. The following columns are displayed:
Flag column
In the example above a yellow flag indicates a warning. Move your mouse over the flag to see the full details. You can also click on the + symbol to the right of the flag and the details will be displayed. This method is useful if you want to print the warning details.
Funder Claim No
This number - allocated by the medical aid - uniquely identifies the specific claim. It can be used in correspondence with the medical aid. It is also displayed on the
eClaims tab
on the Assessment tab at the bottom (Admin. Ref field).
Service date
This is the date the service was provided by the practice, i.e. the Start Date of the
invoice
.
Codes
The BHF codes used in the original claim.
Claimed Amount
The amounts you originally claimed.
Paid Amount
The amounts that will be paid, which may be less than the amounts claimed or even zero if the claim has been rejected. These will be displayed in red when they are less than the amount claimed.
Patient Liable
Amounts in this column are payable by the patient.
Patient Not Liable
Amounts in this column are not payable by the patient. In general you will only see amounts in this column if you have claimed in contravention of a billing arrangement that you have in place with the medical aid, i.e. you have claimed more than the agreed contractual amounts.
Paid To Patient
This column indicates amounts that have been paid to the patient. This sometimes occurs because you have charged more than the medical aid's rate. You will have to claim these amounts from the patient.
Discount
This column indicates discounts that you allowed on your claims.
Reason Codes
This column displays codes that correspond to the reasons displayed at the end of the report. Typically these give reasons for short payment or rejection of claims. You can move your mouse over the code and the reason explanations will be displayed. You can also click on the + symbol in the Reason Codes column and they will be displayed.
|